Many individuals with chronic pain in the pelvis, lower back, or hips may not be aware that the root cause can often be traced back to an issue in the jaw. The relationship between the temporomandibular joint (TMJ) and the pelvis is complex and fascinating, and understanding it can offer valuable insight into treatment options for various types of pain. This article explores the scientific mechanisms behind how tension in the jaw can lead to issues in the pelvis and provides a comprehensive look at why this connection exists.
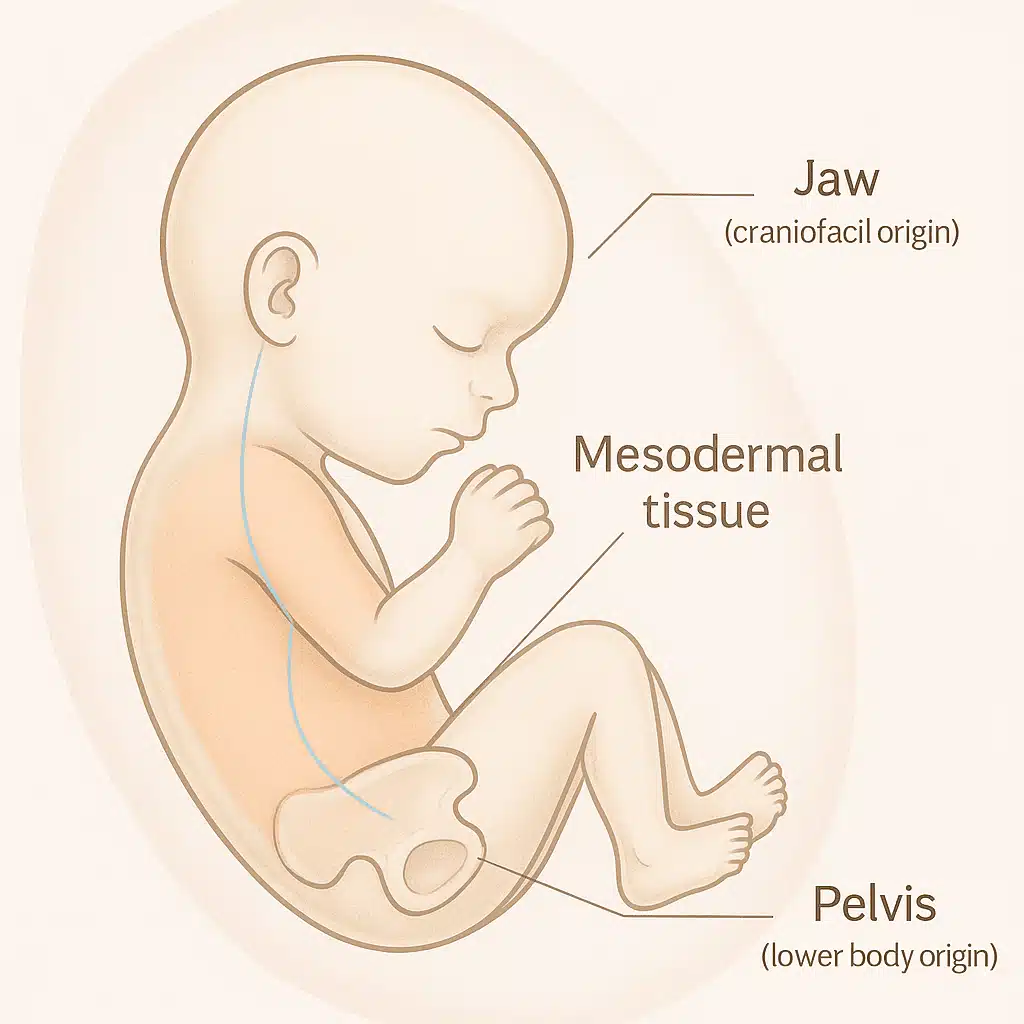
Embryological Origins: How the Jaw and Pelvis Are Connected
The first clue to understanding the jaw-pelvis connection lies in our early development in the womb. During embryogenesis, the jaw and pelvis both originate from the same tissue — specifically, mesodermal tissue. This early shared origin helps explain why issues in one area can sometimes affect the other. The connection doesn’t end with embryonic development; it persists throughout life in the form of shared anatomical and biomechanical patterns.
These patterns can influence how our body moves and how pain manifests. Since both the jaw and pelvis share a similar developmental path, they maintain a functional link even in adulthood. This means that dysfunction in one part of the body — particularly in the jaw — can influence the mechanics of the pelvis, causing pain and discomfort.
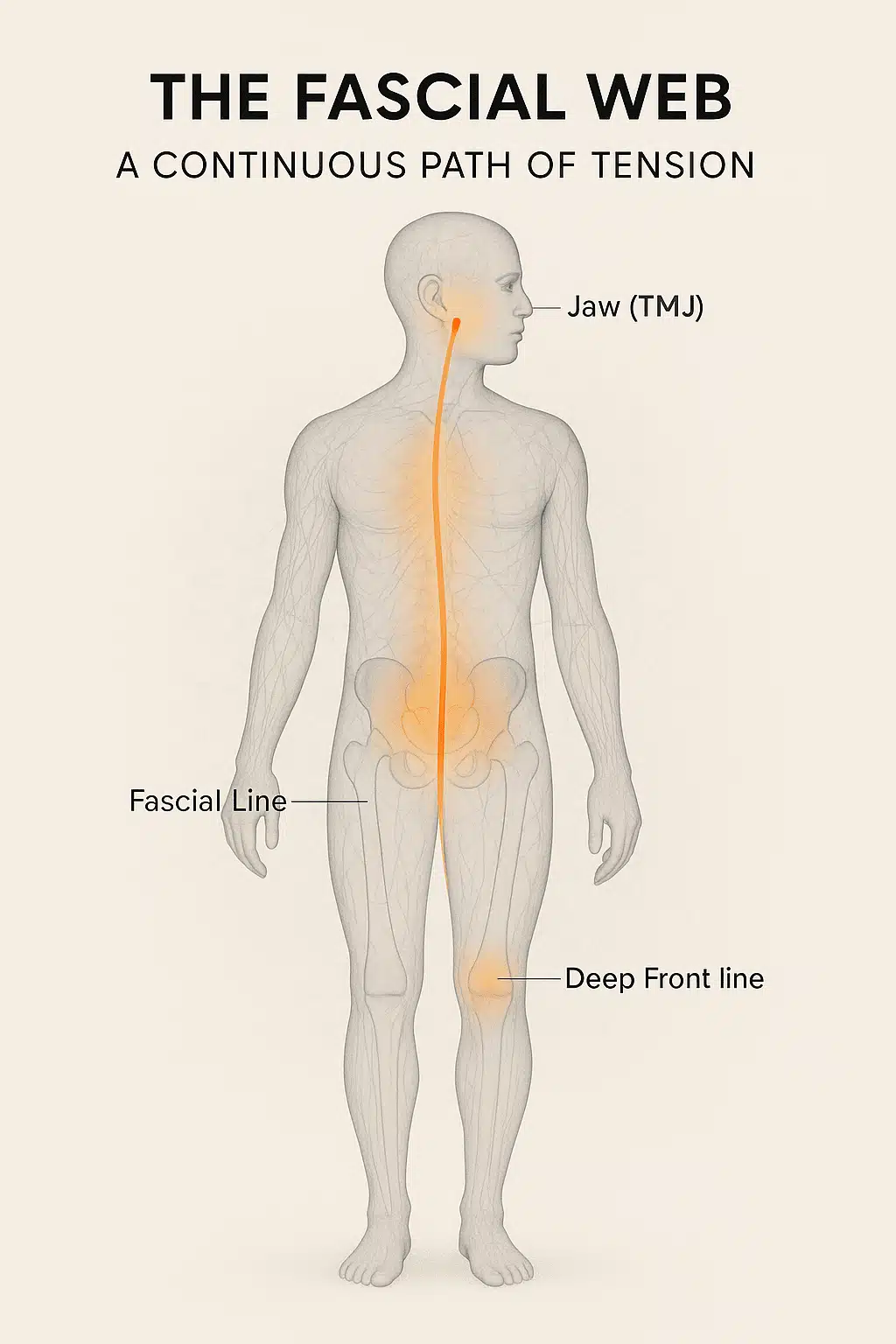
The Fascial Web: A Continuous Path of Tension
One of the most significant pathways connecting the jaw and pelvis is the fascial system. Fascia is a connective tissue that forms a continuous web throughout the body. It surrounds muscles, bones, nerves, and organs, helping them move and function properly. This interconnected tissue acts like a network of highways that transmit mechanical tension and stress throughout the body.
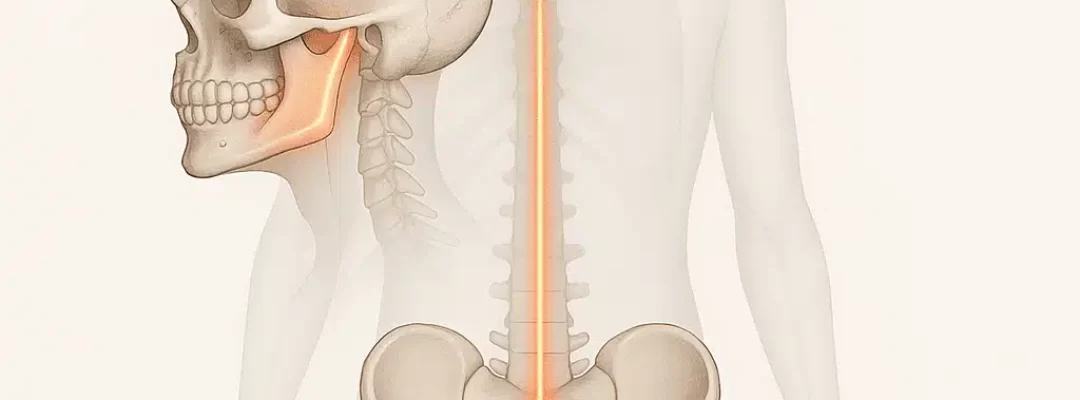
When you clench your jaw or have an issue with your temporomandibular joint (TMJ), the tension in the jaw doesn’t remain isolated. Instead, the tightness and stress are transmitted through the fascial network. A particular fascial line, known as the “deep front line,” runs from the jaw all the way down through the spine and connects to the pelvis.
This is why tightness in the jaw can affect not only the muscles around your head and neck but also the muscles of your lower back, hips, and pelvis. Essentially, a problem that starts in your jaw can cascade down the body, manifesting as pain, stiffness, and tension in the pelvic region. This pathway makes the jaw and pelvis function as parts of an interconnected system, where problems in one area can create symptoms in distant parts of the body.
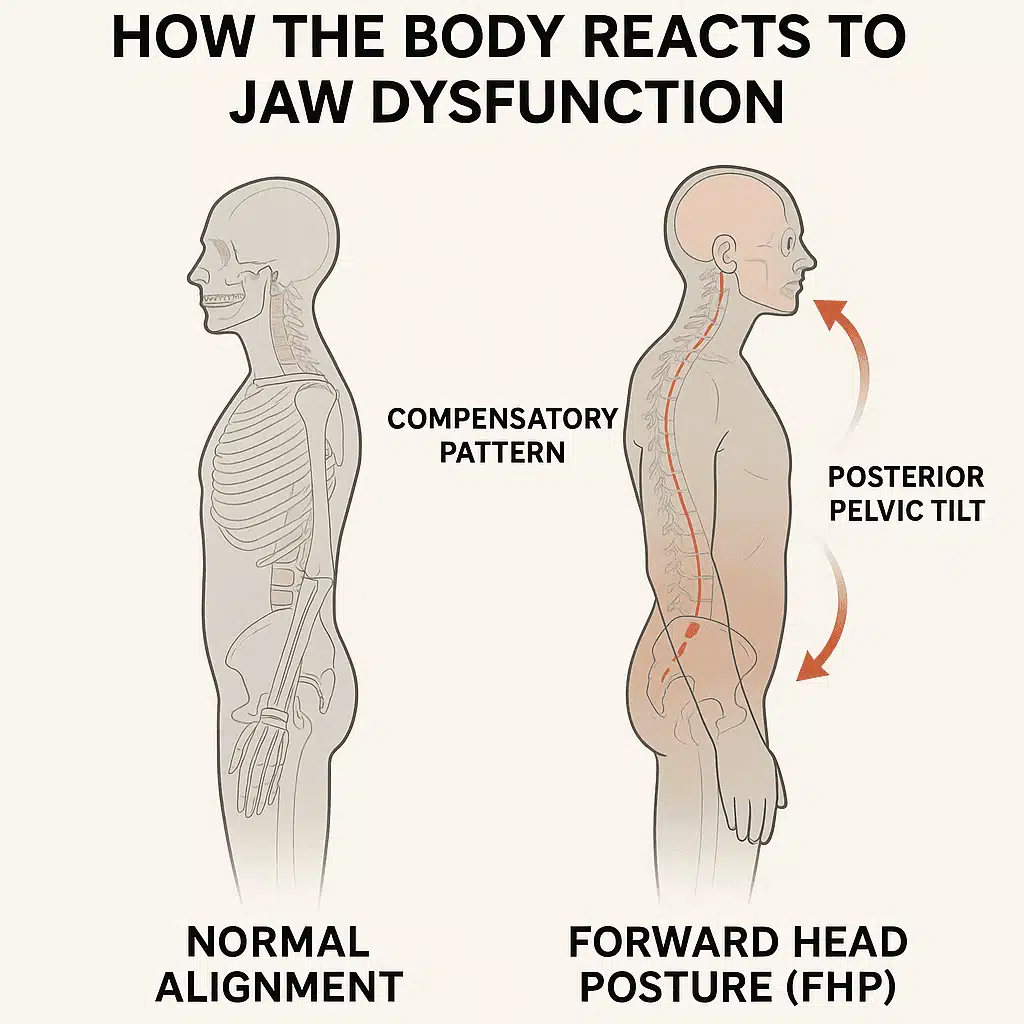
Postural Compensation: How the Body Reacts to Jaw Dysfunction
When TMJ dysfunction occurs — whether due to clenching, grinding, or misalignment — it often causes the head to move forward, a phenomenon known as “forward head posture” (FHP). In a healthy posture, the head should be aligned with the shoulders, but in FHP, the head shifts forward by 2-3 inches or more.
To maintain balance and prevent falling over, the body compensates for the head shift by adjusting the position of the pelvis. The pelvis tilts backward in response, a motion often referred to as “posterior pelvic tilt.” This compensatory action is the body’s attempt to maintain a neutral center of gravity, but it can lead to significant consequences.
The pelvic tilt forces the lower back and sacroiliac (SI) joints to absorb more stress. Over time, this chronic misalignment leads to tightness and pain in the hips, lower back, and even the sacrum. This is why TMJ dysfunction often presents with seemingly unrelated symptoms, like hip pain or sciatic nerve discomfort. The pelvis’s compensation is essential in maintaining balance, but it places undue strain on the body.
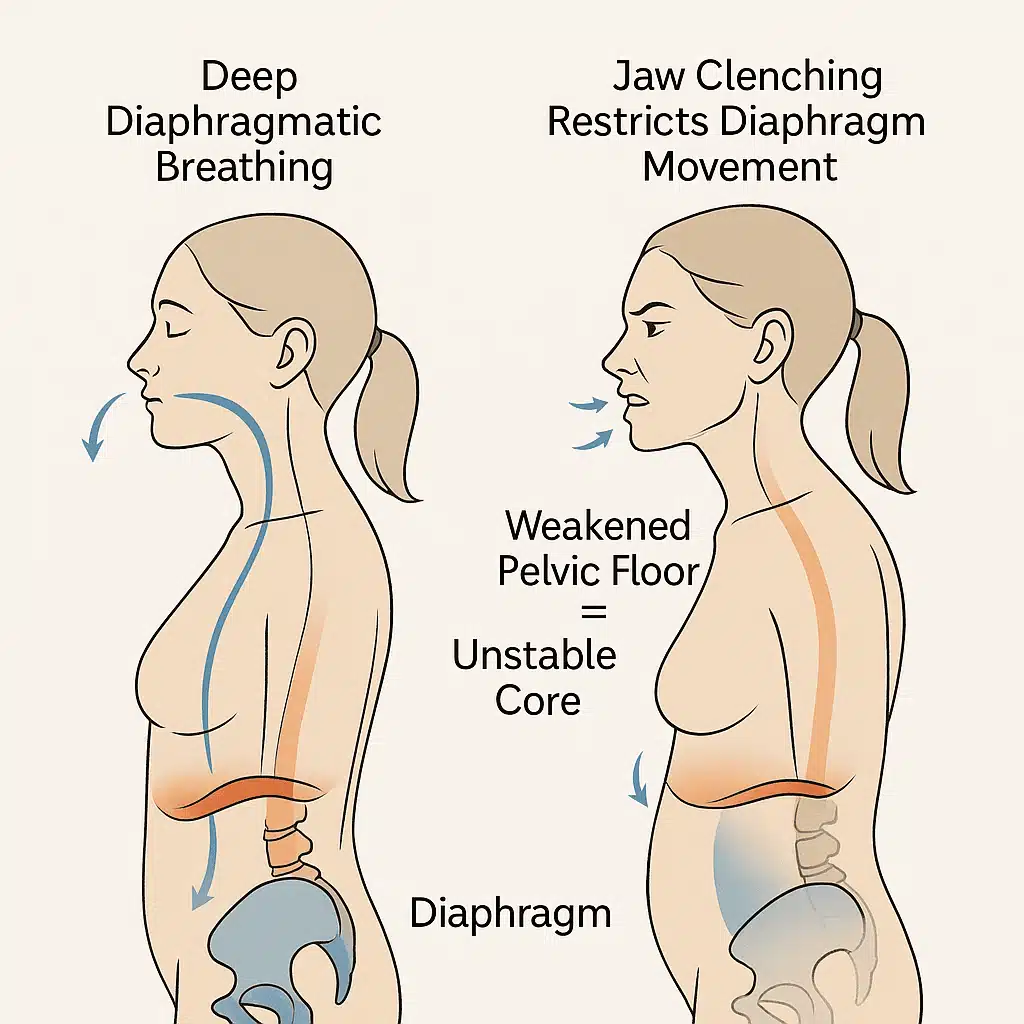
The Breath-Pain Cycle: How Jaw Clenching Affects Core Stability
Jaw clenching doesn’t only affect muscles and joints. It can also interfere with one of the most vital physiological functions — breathing. Normally, breathing involves a deep, diaphragmatic breath where the abdomen rises and falls with each inhalation and exhalation. This breathing pattern engages the diaphragm and supports the pelvic floor muscles, which play a crucial role in core stability.
However, when the jaw is clenched, it can restrict the movement of the diaphragm. This results in shallow, chest-based breathing, which not only limits oxygen intake but also weakens the pelvic floor muscles over time. The pelvic floor is essential for stabilizing the core, supporting the organs, and maintaining overall postural alignment. When these muscles become weak, they contribute to instability in the core, affecting the spine, pelvis, and lower limbs.
A weakened pelvic floor leads to poor posture and chronic pain. Without proper pelvic floor strength, the core muscles are less effective at maintaining balance, causing the hips, lower back, and pelvis to compensate further. This cycle of poor breathing, weakened pelvic floor, and compensatory movements exacerbates the symptoms, creating a vicious cycle of pain.
The Compensation Patterns and Chronic Pain
When TMJ dysfunction forces the head forward, it also changes the distribution of forces across the body. The jaw’s position affects the muscles and structures involved in movement, so a misaligned jaw may lead to postural compensation throughout the entire musculoskeletal system. For instance, tightness in the jaw muscles can affect the muscles around the neck, shoulders, and upper back, leading to discomfort and poor posture.
To prevent falling over, your pelvis will shift backward as mentioned earlier. But this doesn’t just affect the pelvis — it influences the entire kinetic chain, which includes the spine, hips, and legs. The adjustments needed to compensate for head misalignment can cause pain and tension in the hips, lower back, and knees, often leading to chronic conditions like sciatica or pelvic pain.
Chronic discomfort results when the body remains in a state of misalignment for extended periods. The key to managing these pain patterns lies in recognizing and addressing the underlying jaw dysfunction. The jaw doesn’t exist in isolation from the rest of the body; it is part of a dynamic system of interconnected structures that must be in balance for optimal function.
Practical Strategies for Addressing the Jaw-Pelvis Connection
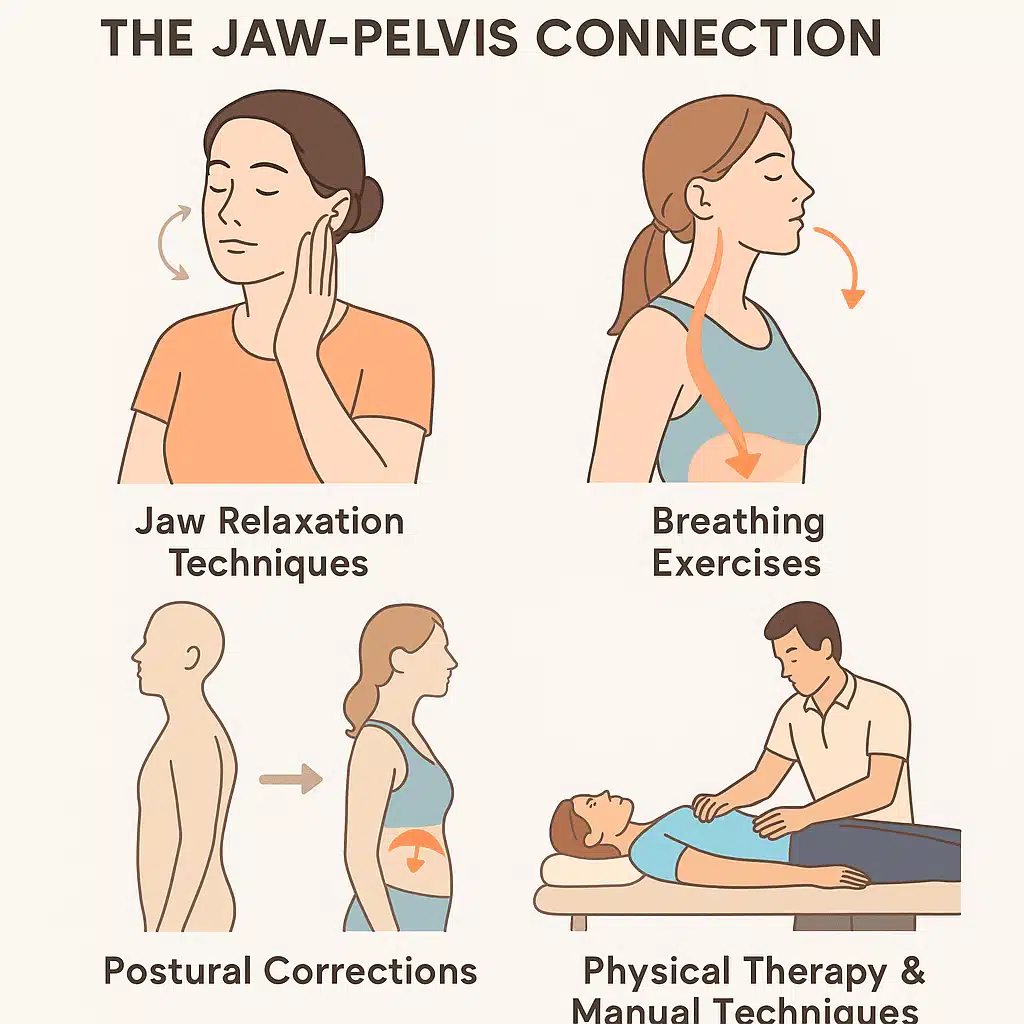
Addressing this jaw-pelvis connection requires a multi-faceted approach that targets both the jaw and the body as a whole. Here are several strategies that can help break the cycle of pain and restore balance:
Jaw Relaxation Techniques
- TMJ Exercises: Gentle jaw mobility exercises and stretching can help relax the jaw muscles and relieve tension.
- Massage Therapy: Trigger point therapy or myofascial release for the jaw and neck can release tightness in the fascial network.
- Jaw Alignment: Consulting a dentist or orthodontist for mouthguards or treatments to align the jaw can help prevent clenching and grinding.
Breathing Exercises
- Diaphragmatic Breathing: Training to breathe deeply with the diaphragm can strengthen the pelvic floor and restore proper core stability.
- Postural Awareness: Ensure that your breathing is not restricted by poor posture. Maintaining spine alignment and keeping the chest open can facilitate better airflow.
Postural Corrections
- Head Positioning: Pay attention to your head position throughout the day. Maintaining a neutral and aligned head position with the spine can help prevent forward head posture.
- Pelvic Alignment: Exercises that focus on pelvic tilts and core stabilization can help restore balance in the pelvis and prevent excessive strain on the lower back.
Comprehensive Physical Therapy
- Myofascial Release and Osteopathy: Manual therapies such as myofascial release, craniosacral therapy, and osteopathy can help address the tension between the jaw and pelvis.
- Chiropractic Adjustments: Some people find relief from spinal misalignments that stem from jaw dysfunction through chiropractic care.
The Neurological Connection: How the Nervous System Links the Jaw and Pelvis
In addition to the anatomical and postural connections, the nervous system also plays a crucial role in the relationship between the jaw and pelvis. The central nervous system (CNS), which includes the brain and spinal cord, coordinates signals from various parts of the body. These signals are processed and interpreted, influencing how the body moves, reacts to pain, and adapts to imbalances.
The trigeminal nerve, which controls the muscles of the jaw, also has connections to other areas of the body through the spinal cord. This nerve is the largest of the cranial nerves and has branches that extend to the face, head, and neck. Interestingly, the trigeminal nerve also shares pathways with nerves that influence the pelvis and lower back.
When the jaw is under stress, such as in TMJ dysfunction or chronic clenching, the trigeminal nerve becomes overstimulated. This overstimulation can lead to referred pain and tension in other areas of the body, including the hips, lower back, and pelvis. In other words, signals from the jaw may travel through the nervous system and manifest as discomfort in distant parts of the body.
Furthermore, the sympathetic nervous system (SNS), which controls the body’s “fight or flight” response, can become activated due to chronic stress. This heightened state of alertness leads to muscle tension, including in the jaw, and can further exacerbate postural imbalances and pain in the pelvis.
Understanding the neurological connections between the jaw and pelvis allows for better-targeted interventions. Techniques that calm the nervous system, such as relaxation practices, deep breathing, and mindfulness, can help alleviate the tension in both the jaw and the pelvis, promoting overall body harmony.
TMJ Dysfunction: A Root Cause of Widespread Pain
TMJ dysfunction is a condition where the temporomandibular joint — the hinge connecting the jaw to the skull — does not function properly. This can be due to a variety of factors, including injury, misalignment, stress, or even bruxism (teeth grinding). Symptoms of TMJ dysfunction often include jaw pain, headaches, difficulty chewing, and popping or clicking sounds in the jaw.
However, the effects of TMJ dysfunction can extend far beyond the jaw itself. As mentioned earlier, the tension in the jaw and head can trigger compensations throughout the body. This is particularly true when the head shifts forward to compensate for jaw dysfunction. The body adjusts by recruiting other muscles to maintain balance, leading to pain and tension in the neck, shoulders, lower back, and pelvis.
People with TMJ dysfunction often find that traditional treatments focusing only on the jaw do not fully address their pain. For this reason, it’s essential to take a holistic approach that not only addresses the jaw but also considers the broader postural and muscular changes that are occurring throughout the body.
The Role of Physical Therapy in Restoring Balance
Physical therapy can be an invaluable tool for managing and addressing the connection between the jaw and pelvis. A skilled physical therapist will assess your posture, movement patterns, and alignment to identify the areas of tension that are contributing to your pain. They will also help you restore balance through targeted exercises and manual therapies.
Jaw-Specific Therapies
A physical therapist may use techniques such as myofascial release or deep tissue massage to relax the muscles around the jaw. Stretching exercises and jaw mobilization techniques can help reduce tension in the temporomandibular joint. Soft tissue work around the neck and head may also be beneficial to alleviate referred pain that radiates down the body.
Pelvic and Postural Alignment
Physical therapy often includes exercises to strengthen the core and pelvic floor muscles, which are critical for maintaining proper posture and alignment. The therapist may use techniques like pelvic tilts, core stabilization exercises, and strengthening of the lower back and abdominal muscles. These exercises help to realign the pelvis, reduce tension in the lower back, and prevent further compensatory shifts.
A therapist may also provide education on proper posture during daily activities. Many individuals with TMJ dysfunction unknowingly exacerbate their symptoms by maintaining poor posture, such as slouching or forward head posture. Physical therapy can teach you how to maintain a neutral spine and head position, reducing the strain on your body.
Psychological Factors and Stress Management
Stress is a major contributing factor to TMJ dysfunction and its subsequent impact on the pelvis. When you are stressed, the body naturally tenses up, and this can lead to clenching of the jaw and poor posture. The jaw muscles are particularly susceptible to stress-related tension, and over time, this can contribute to TMJ dysfunction.
Moreover, the pelvic floor muscles can also be affected by stress. These muscles are often the first to respond to emotional tension, and prolonged stress can lead to pelvic floor dysfunction. This dysfunction can manifest as pelvic pain, urinary issues, and sexual dysfunction.
Addressing the psychological component of TMJ and pelvic pain is essential for long-term relief. Stress management techniques, such as mindfulness meditation, progressive muscle relaxation, and cognitive behavioral therapy (CBT), can help reduce the overall tension in the body. By managing stress and addressing emotional factors, you can alleviate some of the muscular and postural imbalances that contribute to both jaw and pelvic pain.
Integrating Holistic Approaches for Long-Term Relief
While physical therapy and psychological techniques are essential for addressing the jaw-pelvis connection, it is important to consider other holistic approaches as well. Integrative treatments, such as acupuncture, chiropractic care, and osteopathy, can help promote overall body alignment and reduce pain. These modalities work by restoring balance in the musculoskeletal system, helping to release tension in both the jaw and pelvis.
Acupuncture for TMJ and Pelvic Pain
Acupuncture is an ancient practice that involves inserting thin needles into specific points on the body to stimulate healing. Research has shown that acupuncture can be effective in treating TMJ dysfunction by reducing muscle tension and promoting the flow of energy (or “qi”) throughout the body. It can also help alleviate pain and inflammation in the pelvis and lower back.
Chiropractic Care
Chiropractors specialize in spinal alignment and can offer valuable treatments for TMJ dysfunction. Misalignments in the spine, particularly in the upper cervical region, can contribute to jaw and pelvic dysfunction. Chiropractors use manual adjustments to realign the spine, which can help alleviate tension in the jaw and pelvis, improving overall mobility and reducing pain.
Embracing a Comprehensive Approach to Pain Relief
The connection between the jaw and pelvis is a complex and often overlooked aspect of chronic pain. By understanding how dysfunction in the jaw can lead to pain in the pelvis, hips, and lower back, individuals can take a more comprehensive approach to managing their pain. A combination of physical therapy, stress management, postural correction, and integrative treatments can help break the cycle of pain and restore balance to the body.
Rather than treating each part of the body in isolation, it is essential to recognize that the jaw, spine, pelvis, and entire musculoskeletal system are interconnected. By addressing the root causes of pain and considering the body as a whole, individuals can achieve long-term relief from chronic discomfort and improve their overall well-being.